In collaboration with The Foundation for Barnes-Jewish Hospital (FBJH), the Washington University Institute of Clinical and Translational Sciences (ICTS) awards 11 investigators as part of the COVID-19 Research Funding Program. These eight-month grants provide critical financial support for COVID-19 translational research with potential direct clinical impact within the next 12 months. All research will be conducted at Washington University in St. Louis or BJC and projects are set to begin on July 1, 2020.
Each award is supported with funding from the Institute of Clinical and Translational Sciences (ICTS) and The Foundation for Barnes-Jewish Hospital (FBJH).
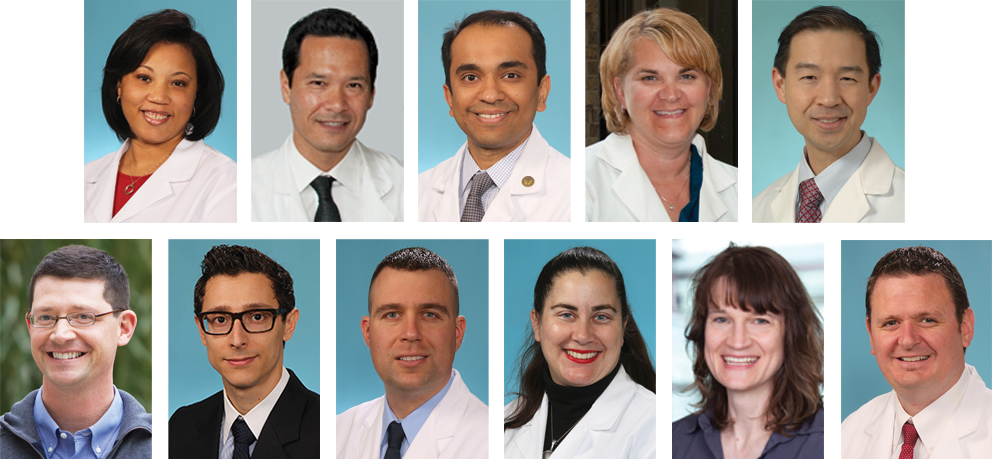
Ebony Carter, MD, MPH, Washington University School of Medicine: Department of Obstetrics and Gynecology – Maternal-Fetal Medicine Division
Although much of the world’s focus is on the lethal respiratory effects of COVID-19, emerging information suggests that COVID-19 puts young women and their babies at increased risk of pregnancy complications. Here, we propose to test the central hypothesis that COVID-19 increases the risks of pregnancy complications through effects on the placenta through the renin angiotensin system.
Andrew Gelman, PhD, Washington University School of Medicine: Department of Surgery – Cardiothoracic Division
Most COVID-19 patients are asymptomatic or only experience mild disease. However, some patients will go onto develop severe respiratory disease leading to death. Recent clinical trials have begun to show some promise through targeting inflammatory cytokine expression and viral replication but are generally considered in patients with advanced COVID-19 disease given their possible detrimental side effects.
Ige George, MD, MS, Washington University School of Medicine: Department of Medicine – Infectious Diseases Division
A recent breakthrough in ultrasensitive fluorescent immunoassays enables the possibility of cheap, fast, simple SARS-CoV-2 antigen testing that is at least as accurate and reproducible as state-of-the-art ELISA. We will develop a test using this technology and evaluate its accuracy on clinical samples (nasopharyngeal swabs and saliva) from patients with COVID-19 disease and compare with current gold standard nucleic acid amplification tests.
Deborah Lenschow, MD, PhD, Washington University School of Medicine: Department of Medicine – Rheumatology Division
SARS-CoV2, the causative agent of COVID-19, has caused significant worldwide social and economic distress. This proposal looks to test two drugs (6TG and 6MP) which are medications currently used to treat cancer to determine if they will be efficacious against SARS-CoV2. We will test these drugs in vitro in human respiratory epithelial cultures and in a new mouse model to determine if they can protect against SARS-CoV2 induced disease.
Stephen Liang, MD, MPHS, Washington University School of Medicine: Department of Medicine – Infectious Diseases Division
While SARS-CoV-2 is transmitted primarily through larger respiratory droplets and direct contact, concern remains that smaller particles (aerosols & droplet nuclei) capable of carrying the virus may be created during patient care and certain procedures. Using air particle monitoring instruments, we will identify whether this is occurring in the emergency department and inpatient settings during acute care, and in dental clinics.
Daniel Marcus, PhD, Washington University School of Medicine: Department of Radiology
The goal of this project is to implement an informatics platform that is engineered to support the development and application of computational imaging algorithms in COVID-19 research, clinical trials, and patient care. The proposed informatics platform will eliminate key barriers – integration of disparate data sources, access to data across institutions, and interfaces to clinical workflows – to developing, validating, and deploying AI applications for COVID-related imaging.
Andrew Michelson, MD, Washington University School of Medicine: Department of Medicine – Pulmonary & Critical Care Division
Recent studies have suggested that a large proportion of COVID-19 patients admitted to the hospital experience a rapid and severe deterioration in their respiratory status. These unanticipated events often lead to delays in care and make resource planning difficult. In this proposal, we are developing a novel machine learning algorithm that can predict respiratory deterioration in COVID-19 patients to facilitate triage and help provide timely and efficient care for our patients.
Philip Mudd, MD, PhD, Washington University School of Medicine: Division of Emergency Medicine
A large proportion of individuals with COVID-19 have severe disease. Many of these individuals require breathing assistance with a ventilator. We have discovered that the level of a few very specific inflammatory blood proteins known as cytokines, measured early in disease, can predict which patients require a ventilator or die. In this grant, we plan to develop a blood test to predict severe disease in patients with COVID-19.
Rachel Presti, MD, PhD, Washington University School of Medicine: Department of Medicine – Infectious Diseases Division
This study will use samples collected from patients who have been infected with SARS-CoV-2, the virus that causes COVID-19. We will look at the immune response over the first year after infection to understand the associations between strong and durable antibody responses and the symptoms and severity of the initial COVID-19 disease. These studies will help us understand who makes good antibodies, how long they last, and how protective they are.
Gwendalyn Randolph, PhD, Washington University School of Medicine: Department of Pathology
White blood cells called monocytes and neutrophils normally protect against pathogens, but sometimes become too active and damage tissues. This study investigates white blood cells collected from patients with mild or extremely severe manifestations of COVID-19. The aim is to understand what processes drive severe disease and then use the information to find ways to interfere with these processes.
Kenneth Remy, MD, MHSc, Washington University School of Medicine: Department of Pediatrics – Critical Care Division
Prolonged hospitalization, secondary infections, and high mortality are hallmarks of COVID-19 disease. An unclear understanding of the immune functional status of COVID patients (i.e.pro-inflammatory or suppressed state) hinders appropriate therapies. We propose a comprehensive evaluation of COVID disease evolution with functional real time immune assays and ex vivo testing of potential immune stimulants for subsequent clinical development.