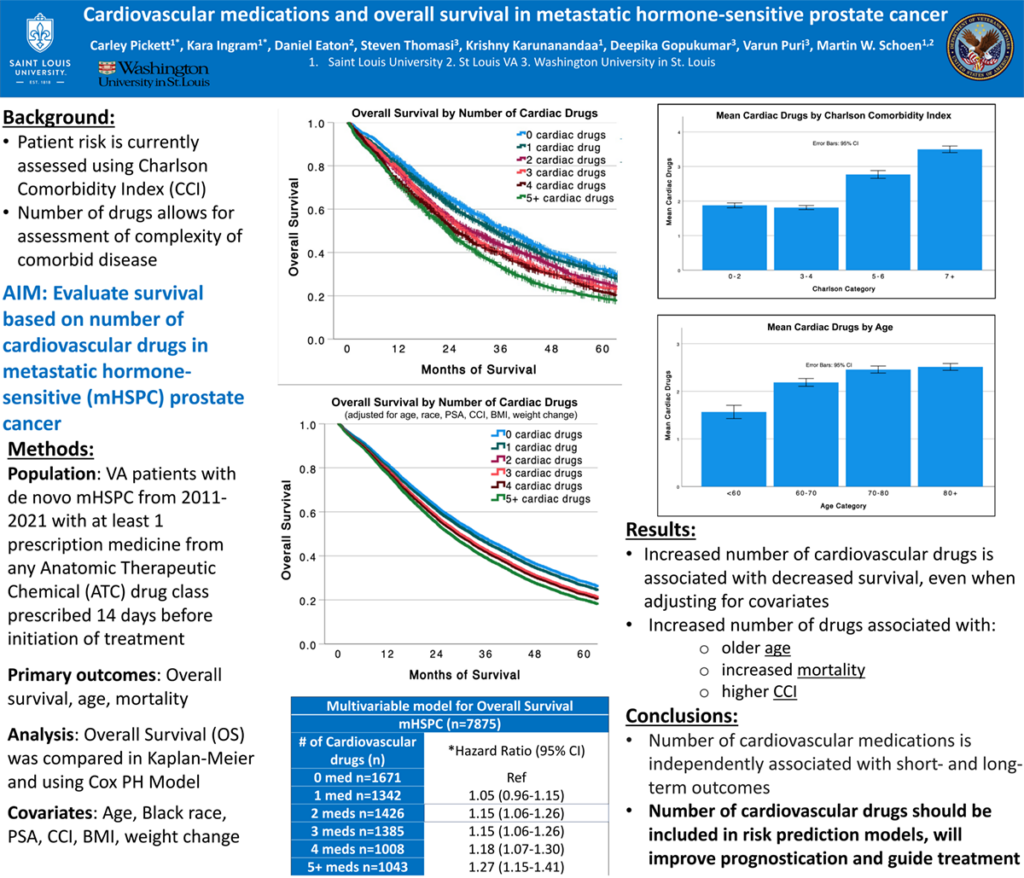
Introduction: Assessment of comorbid cardiovascular disease can predict health outcomes and may risk-stratify patients for adverse events and death. Current methods used to estimate patient risk, such as the Charlson Comorbidity Index (CCI), are based on International Classification of Diseases (ICD) codes, which are a poor indicator of severity and complexity of comorbid disease. In this study, we examined the relationship between cardiovascular medications and survival in patients with metastatic hormone-sensitive prostate cancer (mHSPC).
Methods: In a nationwide retrospective observational study of US Veterans with de novo mHSPC in the VA Health Administration between 2011-2021, we determined the number of cardiovascular drugs prescribed in the year prior up to 14 days before initiation of treatment. Multivariable logistic regression and Cox proportional hazard modeling was used to assess the association between number of drugs with overall survival and mortality.
Results: Among 7,875 veterans, a median of 2 (1-4) unique cardiovascular medications were filled in the year prior to treatment. The mean age was 74 years (SD 10.0) with a median CCI of 3 (3-6). Age was associated with increased number of cardiac medicines (p<0.001). Increased number of medications was associated with decreased OS using the Kaplan-Meier method (p<0.001). The overall survival was 28 months for veterans on 2 medications (aHR 1.15, CI 1.06-1.26), 27 months on 3 medications (aHR 1.15, CI 1.06-1.26), 25 months on 4 medications (aHR 1.18, CI 1.07-1.30), and 23 months on 5+ medications (aHR 1.27, CI 1.15-1.41). After adjusting for age, race, BMI, weight change, PSA, and CCI, the number of medications was independently associated with increased mortality, (aHR 1.05, CI 1.03-1.06) for each additional cardiac medication.
Impact: The number of cardiovascular medications is associated with decreased overall survival and increased mortality in veterans undergoing treatment for mCRPC. Our findings suggest that clinicians can use cardiovascular medications as a simple, reliable tool to estimate comorbid disease and potentially guide treatment discussions in patients with prostate cancer.
Organization: Saint Louis University
Pickett CR, Ingram K, Eaton Jr DB, Tohmasi S, Karunanandaa K, Gopukumar D, Puri V, Schoen MW