Introduction: Pregnant individuals with substance use disorders (SUD) are at higher risk of developing severe complications from COVID-19. Infants < 6 months are also at significant risk. Vaccination in perinatal individuals can help protect both mother and infant from severe outcomes; however, vaccine hesitancy is high. We evaluated COVID-19 vaccination rates among postpartum patients with SUD and identified reasons for vaccine hesitancy.
Methods: Conducted a telephone survey and retrospective chart review in a SUD-specific wraparound perinatal clinic.
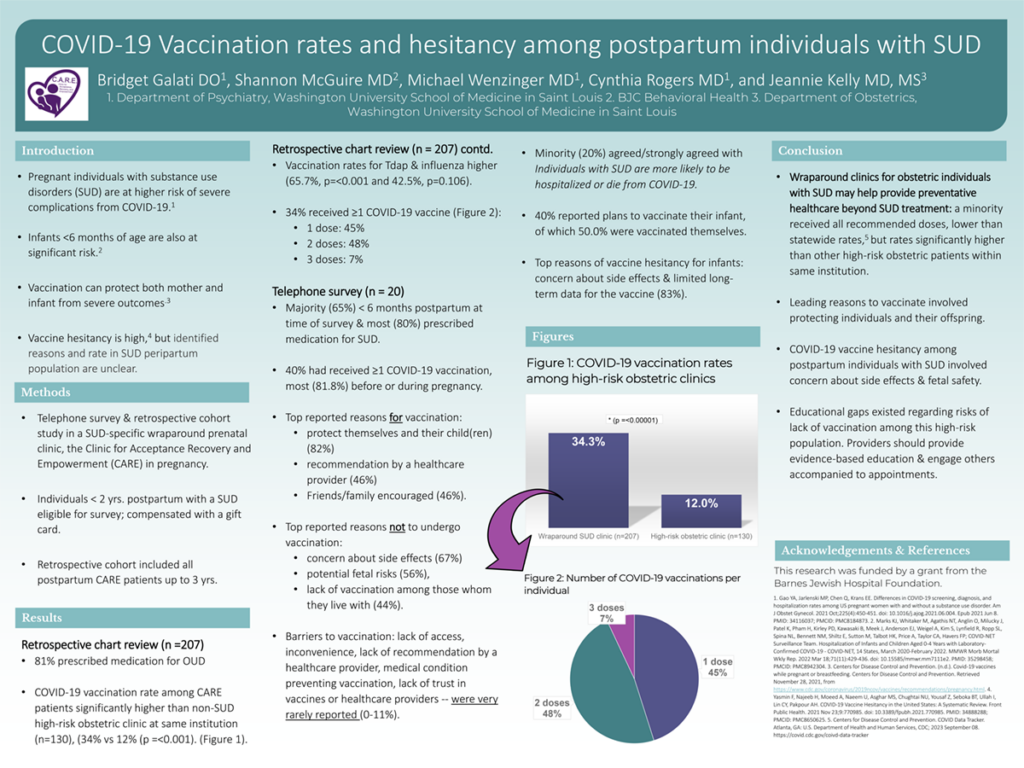
Results: Retrospective chart review included 207 postpartum patients. 80.7% were prescribed medication for SUD. 34.3% had received ≥ 1 COVID-19 vaccination, with 45.1% receiving 1, 47.9% receiving 2, and 7.0% completing 3. Vaccination rates within the past 5 years for Tdap and influenza were higher (65.7%, p=<0.00001 and 42.5%, p=0.105508). COVID-19 vaccination rate was significantly higher than the rate within another non-SUD high-risk outpatient obstetric clinic at our institution (n=130), which had a rate of 12.0% (p =<0.00001). 20 postpartum patients completed the survey, of which 65.0% were < 6 months postpartum. 40.0% received at least one COVID-19 vaccination, most having received vaccination before/during pregnancy (81.8%). Top reason to vaccinate was to protect themselves and their child(ren) (81.8%), followed by provider recommendation (45.5%) and friends/family encouraged vaccination (45.5%). Top reasons not to included concern about side effects (66.7%), potential fetal risks (55.6%), and unvaccinated household (44.4%). Barriers to vaccination – inaccessible, inconvenient, no provider recommendation, medical condition or allergy, lack of trust in vaccines or providers — were very rarely reported (0.0-11.1%). 20.0% strongly/agreed that individuals with SUD are more likely to be hospitalized/die from COVID-19. 40.0% reported plans to vaccinate their infant, of which 50.0% were vaccinated themselves. Top infant vaccine hesitancy reasons included concern about side effects and limited long-term vaccination data (83.3%).
Impact: Wraparound clinics for obstetric individuals with SUD may help provide preventive healthcare beyond SUD treatment.
Organization: Washington University in St. Louis
Galati BM, McGuire S, Wenzinger ML, Rogers CE, Kelly JC