Introduction: Chronic hypertension (CHTN), gestational hypertension (GHTN), preeclampsia (PE), and CHTN with superimposed PE (siPE) are hypertensive disorders of pregnancy (HDP). Criteria distinguishing HDPs are imprecise and the factors driving development of one or more HDPs and progression to PE, associated with increased risk of maternal and fetal morbidity and mortality, are unclear. Identifying more nuanced risk factors and early-warning signs of PE will improve risk stratification of patients, allowing clinicians to implement more intensive monitoring and prophylactic therapies for at-risk patients while reducing unnecessary interventions for low-risk patients.
Methods: We obtained retrospective electronic health records (EHR) data from pregnancy episodes completed between June 1 2018 – August 31 2022 at Washington University/Barnes-Jewish Hospital (BJH) for patients 12-50 years of age. Univariate analyses were performed at the episode-level to identify significant variables associated with PE in individual pregnancies. Geographic information systems (GIS)-based analyses and comparisons of social vulnerability index (SVI) measures were performed at the patient-level to assess the effect of social determinants of health (SDoH) on PE risk.
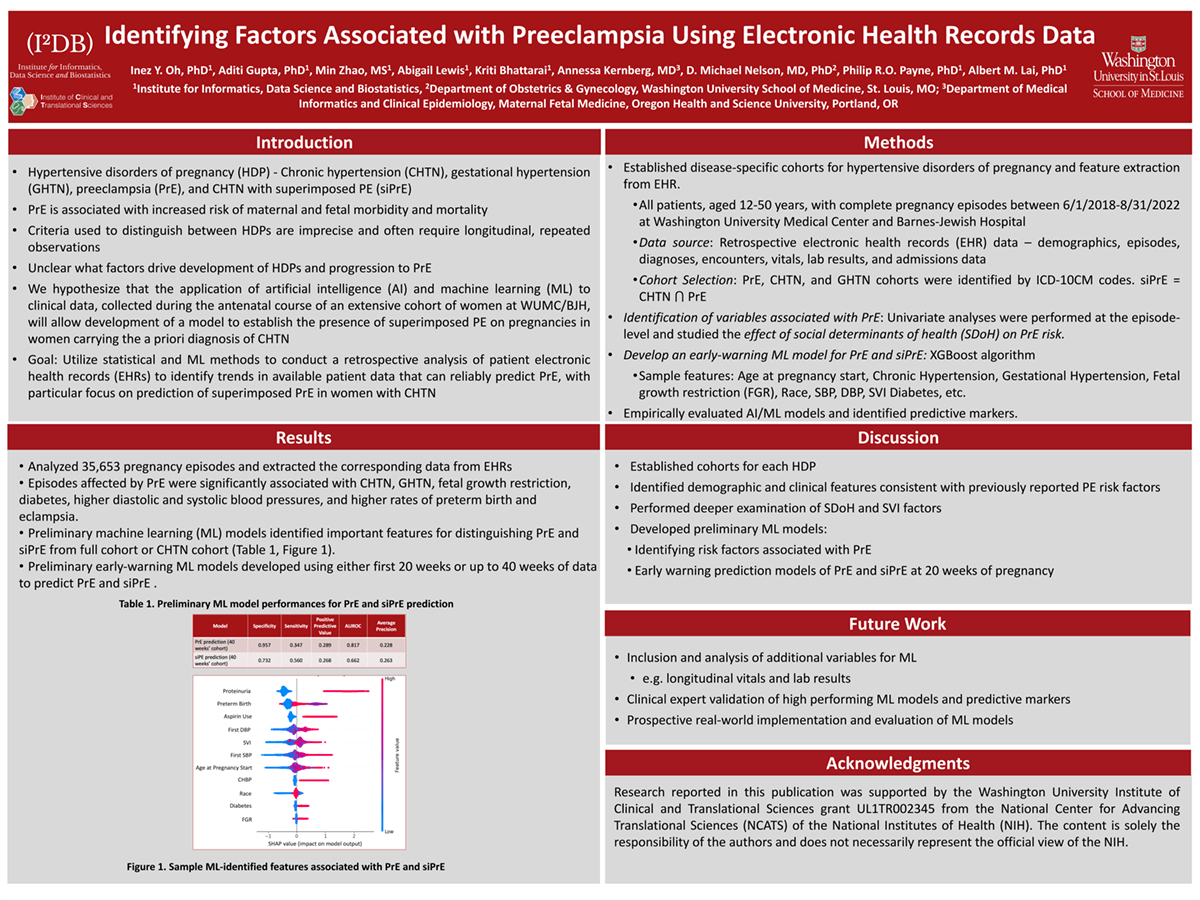
Results: Out of 35,653 episodes, 2,323 (6.5%) were affected by CHTN, 1,511 (4.2%) by GHTN, 1,720 (4.8%) by PE, 340 (1.0%) by siPE, and 30 (0.1%) by eclampsia. Episodes affected by PE were significantly associated with CHTN, GHTN, fetal growth restriction, diabetes, higher diastolic and systolic blood pressures, Black race, and higher rates of preterm birth and eclampsia. 22,472 patients were included in our GIS-based SDoH analyses. Patients who lived further from a prenatal clinic and in disadvantaged neighborhoods had significantly increased odds of developing PE.
Impact: We established cohorts for each HDP and identified demographic, clinical, and SDoH factors that affect PE risk. These are necessary steps towards future development of machine learning models to accurately diagnose and predict development of HDPs, and pinpoint targets for intervention to prevent development of PE and improve PE-related outcomes.
Organization: Washington University in St. Louis
Gupta A, Oh IY, Zhao M, Lewis A, Bhattarai K, Kernberg A, Nelson DM, Payne PRO, Lai AM