Introduction: While internal anal sphincter (IAS) Botox has been increasingly utilized in children with disordered defecation (DD), no literature regarding clinical efficacy or quality of life (QoL) influence exists. Therefore, we aimed to elucidate the effect of IAS Botox as an adjunct to standard treatment for DD on patient/caregiver QoL metrics in association with corresponding clinical outcomes.
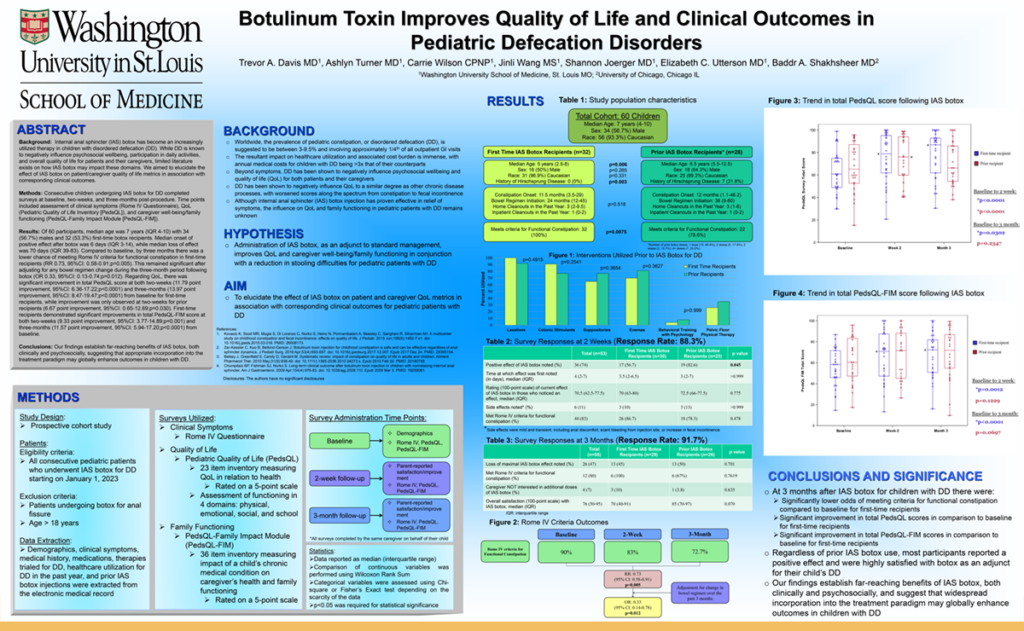
Methods: Consecutive children undergoing IAS Botox for DD prospectively completed surveys at baseline, two-weeks, and three-months post-procedure. Time points included assessment of clinical symptoms (Rome IV Questionnaire), QoL (Pediatric Quality of Life Inventory [PedsQL]), and caregiver well-being/family functioning (PedsQL-Family Impact Module [PedsQL-FIM]).
Results: Of 60 participants, median age was 7 years (IQR 4-10) with 34 (56.7%) males and 32 (53.3%) first-time Botox recipients. Median onset of positive effect after Botox was 6 days (IQR 3-14), while median loss of effect was 70 days (IQR 39-83). Compared to baseline, by three months there was a lower chance of meeting Rome IV criteria for functional constipation in first-time recipients (RR 0.73, 95%CI: 0.58-0.91;p=0.005). This remained significant after adjusting for any bowel regimen change during the three-month period following Botox (OR 0.33, 95%CI: 0.13-0.74;p=0.012). Regarding QoL, there was significant improvement in total PedsQL score at both two-weeks (11.79 point improvement, 95%CI: 6.36-17.22;p<0.0001) and three-months (13.97 point improvement, 95%CI: 8.47-19.47;p<0.0001) from baseline for first-time recipients, while improvement was only observed at two-weeks for prior recipients (6.67 point improvement, 95%CI: 0.65-12.69;p=0.030). First-time recipients demonstrated significant improvements in total PedsQL-FIM score at both two-weeks (9.33 point improvement, 95%CI: 3.77-14.89;p=0.001) and three-months (11.57 point improvement, 95%CI: 5.94-17.20;p<0.0001) from baseline.
Impact: Our findings establish far-reaching benefits of IAS Botox, both clinically and psychosocially, suggesting that appropriate incorporation into the treatment paradigm may globally enhance outcomes in children with DD.
Organization: Washington University in St. Louis
Davis TA, Turner A, Wilson C, Wang J, Joerger S, Utterson EC, Shakhsheer BA