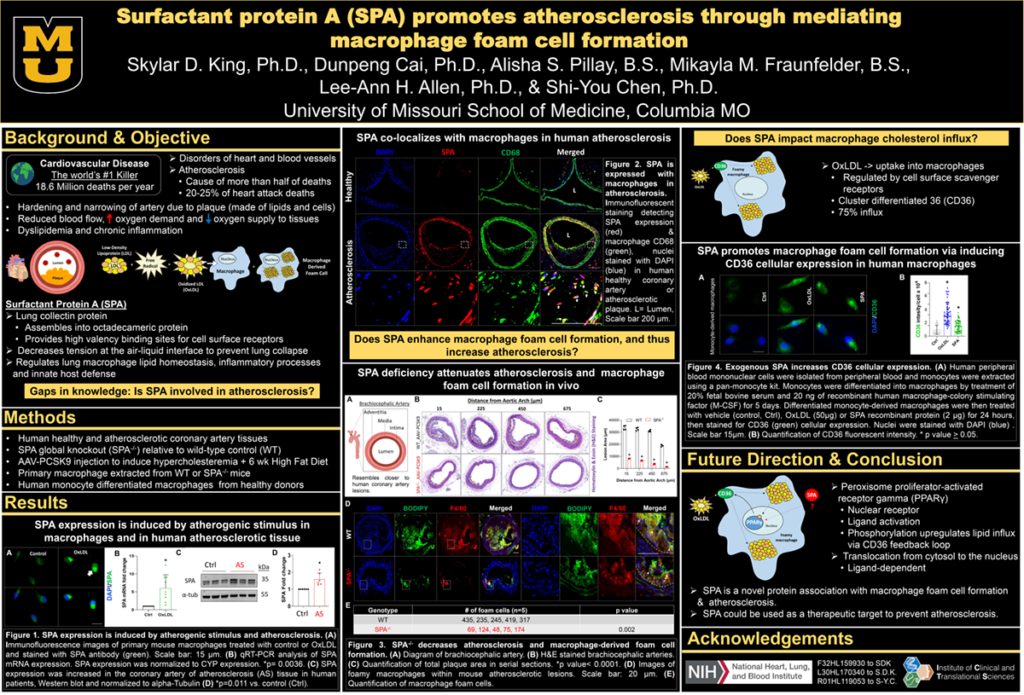
Introduction: Atherosclerosis (AT) is a progressive cardiovascular disease characterized by persistent inflammation and excessive cholesterol deposition within the artery wall and is the fundamental pathological process underlying coronary artery disease and stroke. Macrophage (MФ) foam cells play a central role in the pathogenesis of AT. Surfactant protein A (SPA) is a lipid-associating protein involved with regulating macrophage function in various inflammatory diseases. However, the role of SPA in atherosclerosis and macrophage foam cell formation has not been investigated. Given that AT is associated with dyslipidemia and inflammation, we hypothesized that SPA functions to enhance MФ foam cell formation resulting in increased AT.
Methods: Primary resident peritoneal macrophages were extracted from wild-type (WT) and SPA deficient (SPA-/-) mice to determine the functional effects of SPA in macrophage foam cell formation. SPA expression was assessed after pro-atherosclerotic stimuli in macrophages, in healthy vessels and atherosclerotic aortic tissue from the human coronary artery and WT or apolipoprotein e-deficient (ApoE-/-) mice brachiocephalic arteries fed high-fat diets (HFD) for 4 weeks. Hypercholesteremic WT and SPA-/- mice fed an HFD for 6 weeks were investigated for atherosclerotic lesions in vivo.
Results: In vitro experiments revealed that global SPA deficiency reduced intracellular cholesterol accumulation and macrophage foam cell formation. Mechanistically, SPA-/- dramatically decreased cluster of differentiation antigen 36 (CD36) cellular and mRNA expression. SPA expression was increased in atherosclerotic lesions in humans and ApoE-/- mice. In vivo SPA deficiency attenuated atherosclerosis and reduced the number of lesion-associated macrophage foam cells.
Impact: Our results elucidate that SPA is a novel factor for atherosclerosis development. SPA enhances macrophage foam cell formation and atherosclerosis through increasing scavenger receptor CD36 expression and thus, increasing OxLDL uptake. These findings suggest that the modulation of SPA could be a novel approach for reducing AT.
Organization: University of Missouri – Columbia
King SD, Cai D, Pillay AS, Fraunfelder MF, Allen LH, Chen SY