Introduction: Millions of indwelling catheters are placed each year to monitor urine output. Catheter associated urinary tract infections (CAUTIs) are the most commonly hospital-acquired infections and associated with urinary catheters. Previous efforts to decrease CAUTIs in the intensive care unit (ICUs), which are more likely to use urinary catheters, have had minimal success. Despite unclear indications for use, indwelling catheters may not be removed in patients for various reasons including need for hourly urine output monitoring, limited patient mobility or concern for incontinence. This study seeks to understand the current patterns of and reasons for prolonged catheterization in the surgical ICU. The ultimate goal of the study is to identify ways to decrease urinary catheterization and CAUTIs in the ICU.
Methods: We conducted a retrospective chart review of patients in a 36-bed surgical ICU from 01/01/2022-06/30/2022 who had a urinary catheter placed during admission. We defined the appropriateness of catheterization as correlation between catheter utilization indication versus evidence of such during chart review. Abstractors reviewed records for: insertion details, duration, associated acute kidney injury (AKI), severity of illness, disposition, and mortality. Inter-rater reliability will be described.
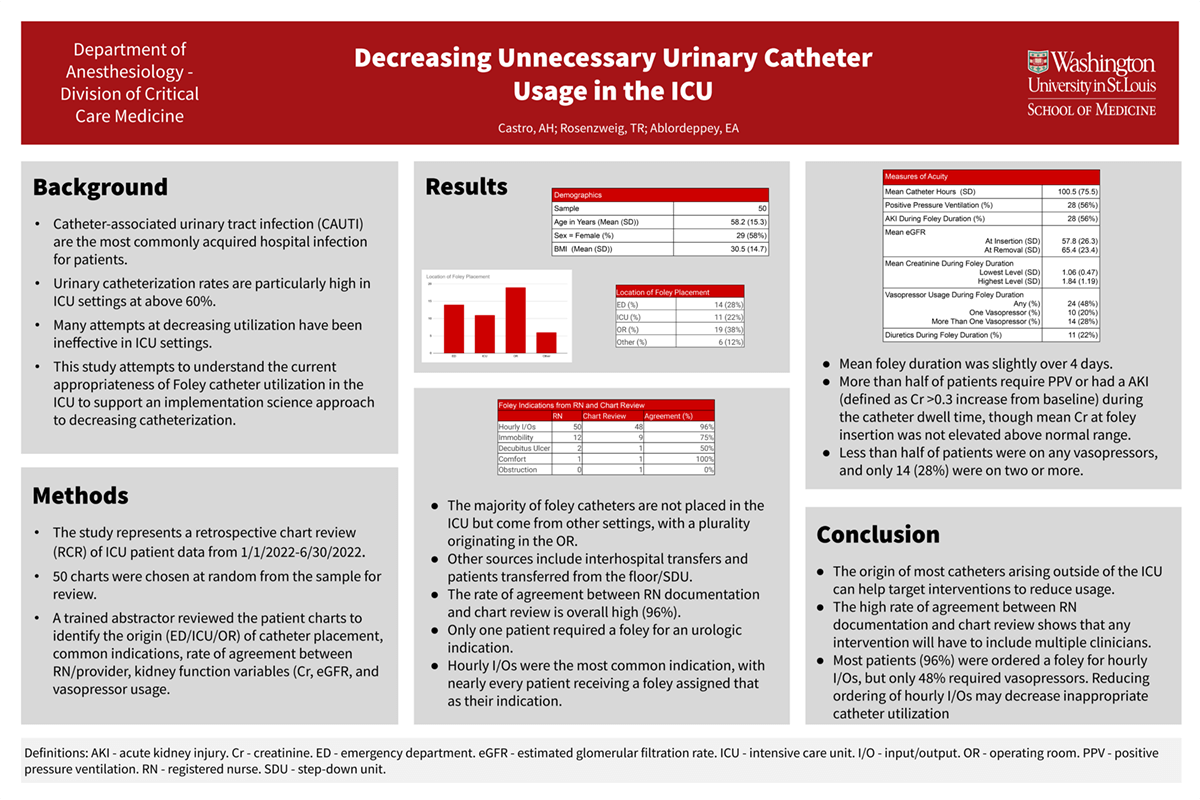
Results: Results will describe current practice patterns of urinary catheterization in the ICU. Data will highlight the relationship between severity of illness, frequency of associated AKI, and urinary catheterization rates. Data will also identify most common urinary catheter placement location (Emergency Department /ICU/Operating Room), average catheter duration, key indicators identified for catheter maintenance, and occurrence of maintenance vs. chart indication.
Impact: The first step to developing an implementation program to decrease unnecessary urinary catheter use is to develop comprehensive understanding of the current practices of urinary catheter utilization in the ICU. Demonstrating a protocol that decreases urinary catheter rates in the ICU would be a significant change in practice and can directly improve patient care outcomes. Decreasing the rates of CAUTIs results in disease prevention and improved health care quality and delivery, while simultaneously resulting in cost savings for the hospital system.
Organization: Washington University in St. Louis
Castro AH, Ablordeppey EA, Rosenzweig TR