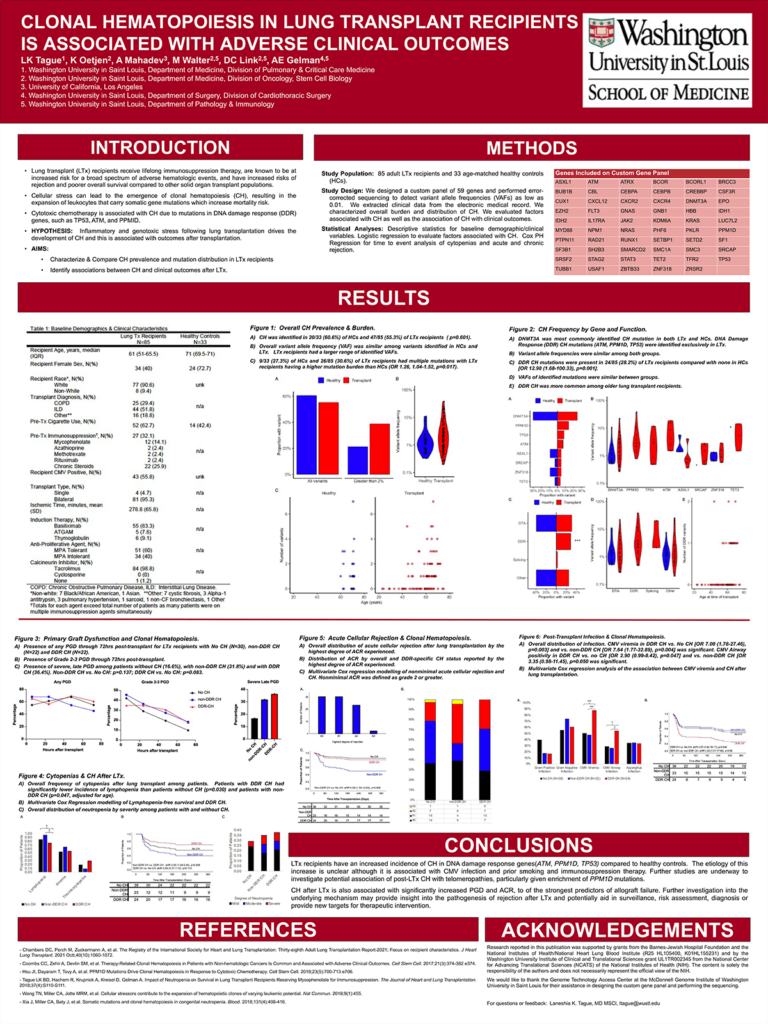
Introduction: Cellular stressors play an important role in the emergence of clonal hematopoiesis (CH). Cytotoxic chemotherapy is associated with CH due to mutations in DNA damage response (DDR) genes, such as TP53, ATM, and PPMID. Lung transplant (LTx) recipients receive lifelong immunosuppression therapy and are known to be at increased risk for a broad spectrum of adverse hematologic events. We hypothesized that, similar to cytotoxic chemotherapy, the inflammatory and genotoxic stress of lung transplantation likewise drives the development of CH.
Methods: We performed a prospective cross-sectional cohort study of 85 adult lung transplant recipients (LTx) and 33 healthy controls (HC) to 1) characterize CH prevalence and 2) identify associations with transplant outcomes. We evaluated CH frequency and burden with chi-square and Poisson regression, associations between clinical and demographic variables and CH using logistic regression, and between clinical outcomes and CH using Cox regression.
Results: CH in DDR genes was more prevalent among LTx (24/85 LTx vs. 0/33 HC, aOR 12.9 (1.7-100.3), p=0.0002). Age [OR 1.13 (1.03-1.25), p=0.014], ILD diagnosis [OR 3.6 (0.9-15.5), p=0.083], pre-transplant smoking (OR 4.25 (1.02-17.82), p=0.048], and mycophenolate intolerance [OR 3.8 (1.3-12.9), p=0.031] were associated with DDR CH. Non-DDR CH was associated with non-minimal acute cellular rejection [aHR 13.9 (3.5-56.2), p=0.0002] and moderate to severe neutropenia [aHR 8.9 (1.2-64.7), p=0.03]. DDR CH was strongly associated with CMV viremia [aHR 4.1 (1.02-16.2), p=0.046].
Impact: Our findings of CH amongst lung transplant recipients represents a potential paradigm shift in how adverse clinical outcomes in solid organ recipients are screened for, evaluated, and possibly treated in the post-transplant population. The potential applications include assessing risk for common hematologic complications, evaluating the potential response to immunosuppressive therapy, risk stratification for the development of rejection and possibly novel immunosuppression agents and therapeutic targets. Future studies are needed to confirm these findings and investigate the underlying mechanisms of these relationships.
Organization – Washington University in St. Louis
Tague LK, Oetjen K, Mahadev A, Link DC, Gelman AE