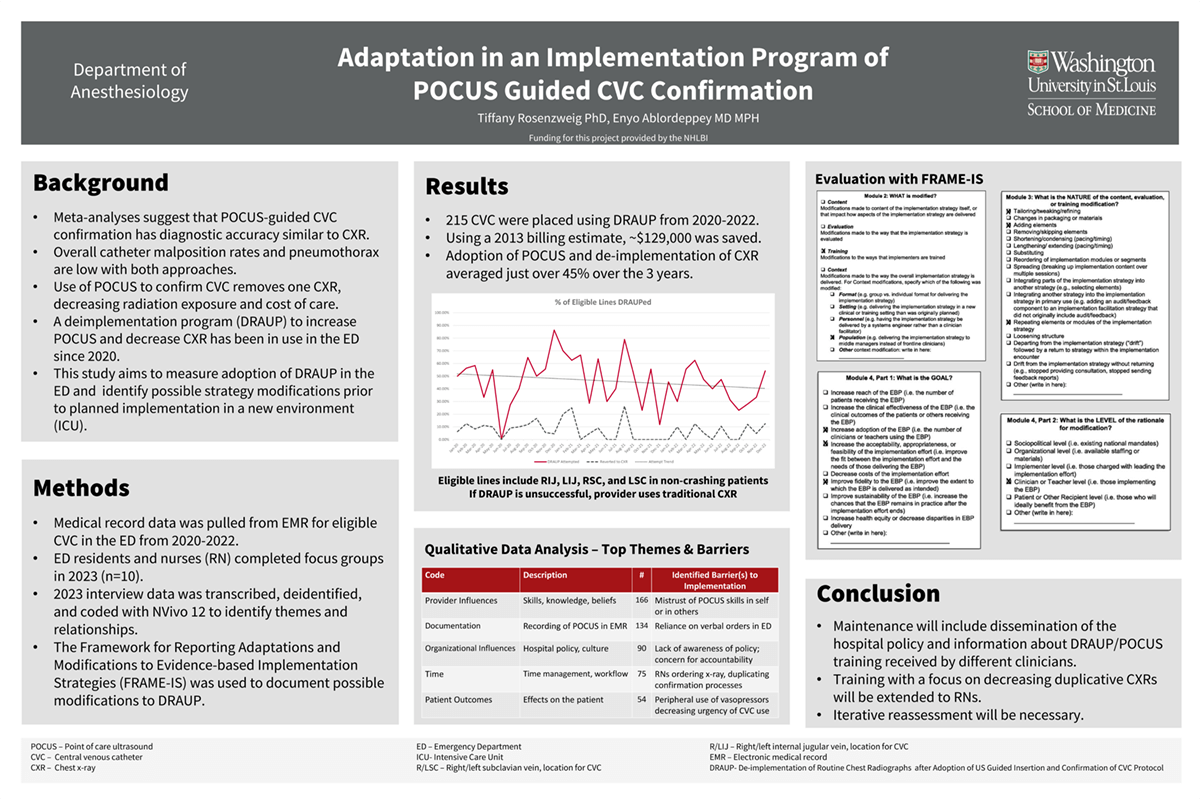
Introduction: Ultrasound (US) guided confirmation of central venous catheters (CVC) has similar sensitivity to the traditional chest x-ray (CXR), while being less resource intensive and lowering labor cost. In spite of this data, clinicians continue to obtain CXR for CVC confirmation and have not adopted US, a new innovation, to replace CXR. A protocol was developed and a deimplementation program [DRAUP] was initiated to increase the use of US guided CVC confirmation in lieu of CXR in the ED. To be generalizable, this study aims to consider sustainability of this deimplementation program by using FRAME-IS conceptual framework to design an adapted and tailored program and rigorously document modifications to implementation strategies. We hypothesize that by using an implementation science approach to determine the types and degree of adaptions, we will determine necessary intervention changes for continued successful adoption of DRAUP.
Methods: Data on the implementation of a program to decrease the use of chest x-rays in CVC confirmation was tracked for 3 years. To explore barriers to continued adoption of the protocol and areas for adaptation, participants completed a short demographics surveys and a moderator led focus group or interview. Interviews will be transcribed and analyzed for major themes using a behavioral theory addressing capacity, opportunity and motivation [COMB]. The FRAME-IS will guide selection and prioritization of adaptation strategies.
Results: The completion of qualitative methods for focus groups and interviews is underway. One adaptation already underway in the program is to better understand the role of RNs in CVC placement. Analysis of the interviews with RNs and physicians in the ED will identify ways to adapt the education and training components of the program.
Impact: The project focuses on changing clinical guidelines for CVC confirmation to support the reported benefits of US. The shift improves healthcare by improving efficiency and resource allocation, decreasing the amount of radiation received by patients during a hospital stay and creating cost savings for both the patient and healthcare system.
Organization: Washington University in St. Louis
Rosenzweig TE, Ablordeppey AE