Introduction: In 2020, suicide was the 12th leading cause of death for people of all ages in the United States (US), the second leading cause of death for people, aged 10 to 34, and the fifth leading cause of death for people aged 35 to 54 (Garnett et al., 2020). Despite prevention and treatment efforts, research on healthcare contacts shows that 83% of patients saw a primary care provider (PCP) within one year of suicide death (Ahmedani et al., 2014). Considering barriers to specialty mental health services and the prevalence of PCP management of patient mental health conditions like depression, there is demand for physicians to be equipped with tools to identify, assess, and refer patients at-risk for suicide (Bono & Amendola, 2015). Behavioral health integration is a dynamic approach that seamlessly integrates both mental and physical health services such as same-day warm handoffs to behavioral health consultants, or regular consults with psychiatry (Curtis and Christian, 2012). The aim of this quantitative research study was to evaluate the relationship between level of behavioral health integration and PCPs’ self-reported beliefs about knowledge and confidence regarding suicide risk reduction activities.
Methods: Primary Care Providers (n=233) in the US were invited to participate in a 35-item electronic survey adapted from the Zero Suicide Workforce Survey to assess knowledge and confidence about suicide, as well as questions about collaboration with behavioral health clinicians.
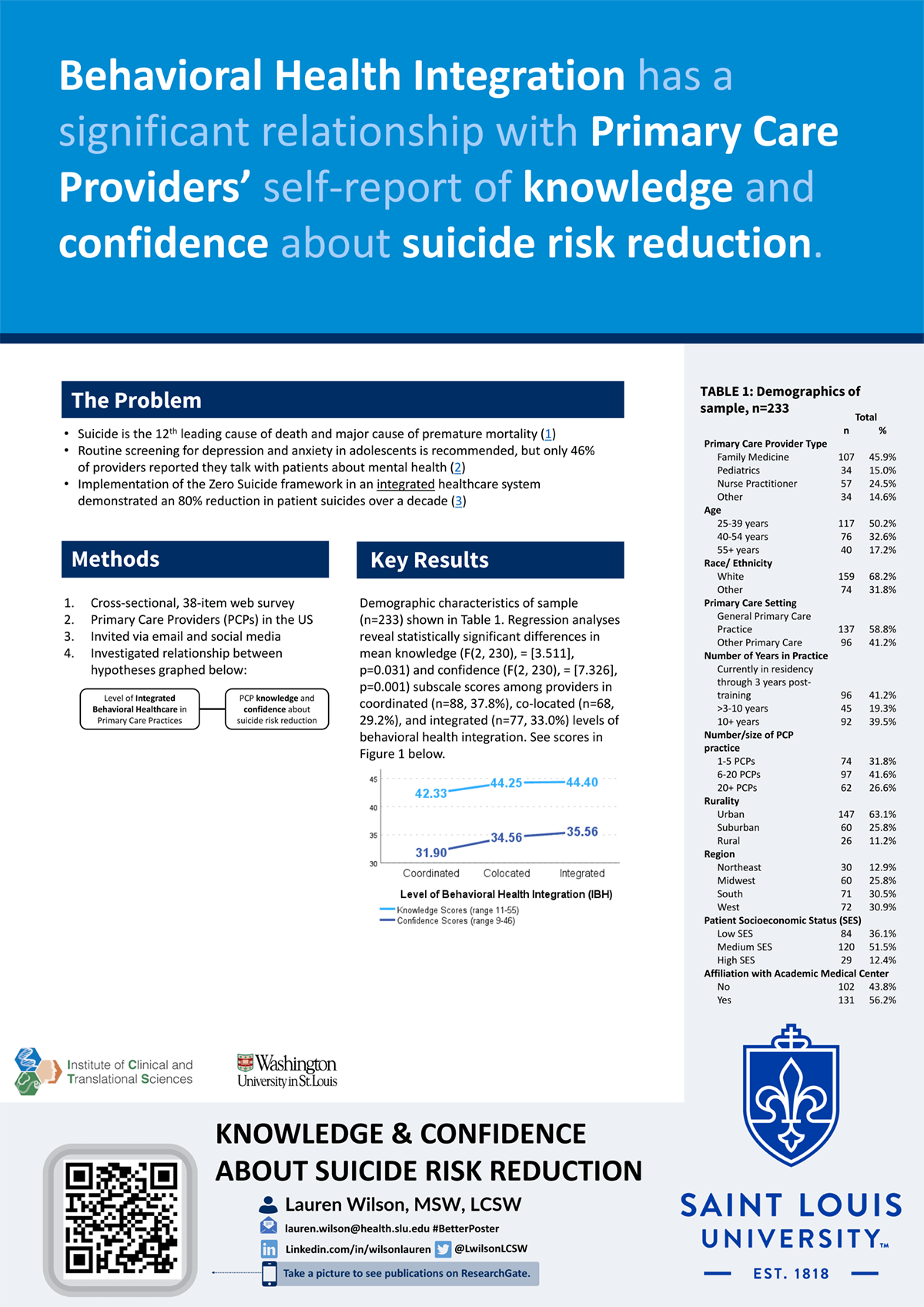
Results: Differences in mean knowledge (F(2, 230), = [3.511], p=0.031) and confidence (F(2, 230), = [7.326], p=0.001) subscale scores were statistically significant among providers in coordinated (n=88, 37.8%), co-located (n=68, 29.2%), and integrated (n=77, 33.0%) levels of behavioral health integration.
Impact: This project has potential community and public health benefits. Health care characteristics that promote behavioral health integration in primary care via patient-centered, collaborative teams has potential to bridge the continuity of care gap and better serve patients and families experiencing suicidality.
Organization: Saint Louis University
Wilson LE