When it comes to pinpointing the best courses of treatment for cancer patients, there is always room for improvement. That has been the belief for two investigators at the Washington University School of Medicine, leading them to the groundbreaking development of a genomic sequencing test that captures a full picture of patient-specific data. This provides crucial information that physicians can use to help determine optimal treatment strategies for individual patients with certain kinds of blood cancers.
In 2021, Eric Duncavage, MD, Professor of Pathology & Immunology, and David Spencer, MD, PhD, Associate Professor of Medicine, published details of their work on Chromoseq, a genome sequencing test for patients diagnosed with Acute Myeloid Leukemia (AML), or a group of blood cancers known as Myelodysplastic Syndrome (MDS). Co-author and team member, Molly Schroeder, PhD, Associate Professor of Pathology & Immunology, provided critical support on the project as Medical Director of the Clinical Genomics Laboratory.
Advancements in Accessibility
The test has been used routinely for a few years by Washington University oncologists, but in August 2023, Chromoseq became the first whole-genome sequencing test for cancer to be approved for reimbursement by the Centers for Medicare & Medicaid Services. This equals far more accessibility, since physicians nationwide caring for Medicare patients diagnosed with AML or MDS will be able to order the test through Washington University Pathology Services, and Medicare will cover the cost.
“Insurance coverage is a big deal,” says Duncavage. “We’ve started to pave the way for other institutions and vendors to get these types of assays approved, and I think it will help drive the overall adoption of the genomic sequencing approach to treatment.”
Chromoseq could also level the playing field for patients who are located in areas where reliable genetic testing methods may not be as easily accessed. Conventional testing methods require skilled technicians to visually examine chromosomes that must be prepared from living cells. Therefore, a patient living in rural Missouri or a place where they don’t have access to a genetics lab that performs this analysis must ship their samples long distance. This can mean the cells may not be adequate for chromosome analysis, and the patients may not get the same type of result that they would if they were having the testing done close to home. Samples taken with Chromoseq, however, require only DNA and not living cells, which is much more stable when transported to clinical testing labs, like the one at WashU. Chromoseq provides the same type of information as chromosome analysis in addition to gene mutation data that is useful for clinical management of patients with these cancers.
“Genomic sequencing allows for the standardized evaluation of patients,” says Duncavage. “Not every facility has the same level of diagnostic care, so depending on where the patient goes and is diagnosed, they will get a different workup using the more conventional methods of testing. But this genomic sequencing is a single assay, and everyone gets the same complete evaluation, which increases the probability of finding a variant in their cancer that could potentially change their course of treatment.”
Improvements in Precision
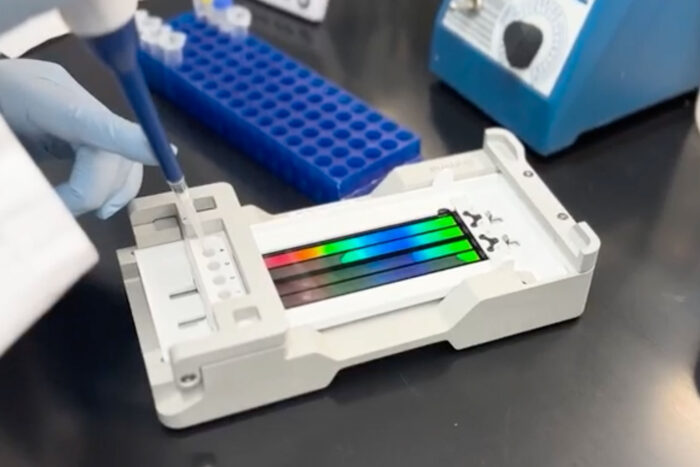
In addition to accessibility, Chromoseq makes the testing results more accurate. This type of patient-specific data has historically been collected through labor-intensive microscopic examination of chromosomes, and other assays that test for specific gene mutations. The results from many tests then must be assembled make the correct diagnosis and decide on the appropriate treatment for patients. Chromoseq provides all this information in a single test, making it more streamlined and convenient for oncologists.
“Many tests are performed and they all need to be collected together to make a complete genetic report for each patient. Sometimes the testing for mutations in these cancer patients is incomplete, and some of the conventional methods are not terribly precise,” said Spencer. “In fact, we’ve found that 10-20% of patients using conventional testing methods have something happen where the full spectrum of mutations is not captured. We saw this as an opportunity for improvement, and developed a test using whole-genome sequencing in a fast and streamlined way so all of the necessary genetic information can be summarized in a single report.”
Chromoseq is also getting genetic results into the hands of patients and physicians in a more consistent and timely fashion. Spencer points out that while other testing methods can take up to 3 weeks at times to get results, depending on how well the cells grow and how complicated the sample is to interpret, Chromoseq is subject to much less variability in turnaround time that allows for a shorter duration in which patients and physicians have to wait before making treatment decisions. That can make a difference for some time-sensitive cancer therapies.
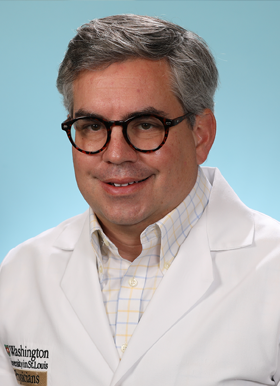
“We’ve been doing genetic analysis on these cases for years, but the conventional technology goes back to the late 1950’s,” says Duncavage. “What other technologies have persisted for so long? This is like “rotary phone” era technology that we are bringing into the 2024 era of single-base resolution. It is a big step forward in terms of us understanding the human genome and how it impacts patient care.”
Examples of Efficiency and Real Successes
In their 2021 published study, the team was able to demonstrate the effectiveness of Chromoseq on nearly 300 patients. Spencer says that the genomic sequencing performed by Chromoseq identified several mutations that were missed by conventional testing methods.
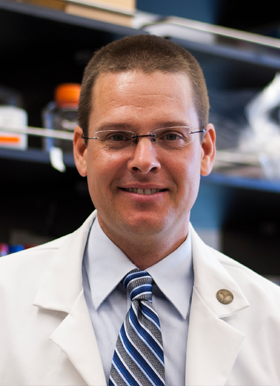
“In some of these cases where genomic sequencing was performed, the patient was known to respond poorly to chemotherapy,” indicates Spencer. “So these findings that would not have been detected using conventional testing methods could have helped the clinicians make clinical decisions or understand treatment responses for individual patients.”
Spencer adds that the next open question is whether findings identified by Chromoseq directly impact and modify the treatment and management of patients. There is an ongoing clinical study working to answer that important question.
Support from the ICTS and WashU
Chromoseq development has benefited directly from ICTS funding, with a Clinical and Translational Research Funding Program (CTRFP) award for Duncavage in 2015 and a CTSA Supplement award for Spencer in 2018. Duncavage is also a current awardee of the CTRFP, where his project focuses on advancements in technology that allow for more long-read sequencing, which Duncavage says makes it easier to see the more complicated regions of the genome.
In addition to funding opportunities, Spencer says being part of an institution where translational work is valued is vital to the success of projects like the development of Chromoseq.
“I have a research lab that is focused on basic science,” said Spencer. “The development of ChromoSeq was a translational science project–a good idea that can improve aspects of medicine and advance human health. Having access to the ICTS that is focused on the science of translation was critical. The funding and support provided by ICTS was really beneficial for our projects and others like it in the future.”

Recently, the ICTS worked with Duncavage and Spencer on a case study and impact profile using the ICTS-developed Translational Science Benefits Model, highlighting the evolution of Chromoseq. TSBM case studies showcase the real-world impact of translational science projects like this one and how they affect human health in the Clinical, Community, Economic, and Policy domains. For example, the case study identified demonstrated benefits in Clinical testing guidelines and in Economic cost savings for reduced testing costs and insurance coverage. Potential Community benefits may be even more far-reaching, leading to enhanced health care accessibility and care quality as well as improved life expectancy and quality of life.
Home of the Genome
Spencer points out that this project is the culmination of the Human Genome Project and all the research that’s gone into human genomes in the last 30 years.
“We developed a test to do whole-genome sequencing on cancer patients in a routine way, which was possible because of the Human Genome Project.”, says Spencer. “We’ve benefited from the work done at WashU and in labs across the world that has advanced the tools, technologies, and our fundamental understanding the human genome.”
Duncavage credits reaching the Chromoseq milestone and roll-out before other labs because of the rich resources here at WashU. In fact, he likes to think of WashU as the “home of the genome”.
“This is something that WashU has had a big impact on over the years, from sequencing the very first cancer genome to now sequencing the genomes of our cancer patients to make treatment decisions, which has always been the promise of precision medicine, but it’s taken a lot of resources to make it happen,” says Duncavage.
Looking Forward
Duncavage says that he believes in the next 3-5 years, we will transition away from looking at DNA under the microscope to more widely using these advanced sequencing methods.
“Cancer is a disease of the genome, and over time, our testing will start to reflect that fact,” says Duncavage. “A lot of what we do in pathology now is looking at cells under a microscope as we have for the last 100 years, but as sequencing methods have evolved, pathology will transition to the genomics era. Right now, we’re just at the tip of the iceberg.”