Introduction: Most dementia patients have co-existing vascular contributions to cognitive impairment and dementia (VCID). Cerebral amyloid angiopathy (CAA), a form of vascular dementia, bridges the interplay between VCID and Alzheimer’s Disease (AD) pathology and cooccurs in 90% of patients with AD. The hallmark pathology of CAA is characterized by amyloid-ß deposition in cerebrovasculature. Reactive oxidative species (ROS) promotes vascular oxidative stress (VOS) in CAA. It is now known that NADPH oxidase-derived VOS is a critical mediator of cerebrovascular dysfunction in CAA. Further, Heparan sulfate proteoglycans (HSPGs) are understood to be responsible for the upstream molecular initiation governing Aß induced oxidative stress and vessel dysfunction. Translational evidence does not yet exist associating these molecular markers with CAA.
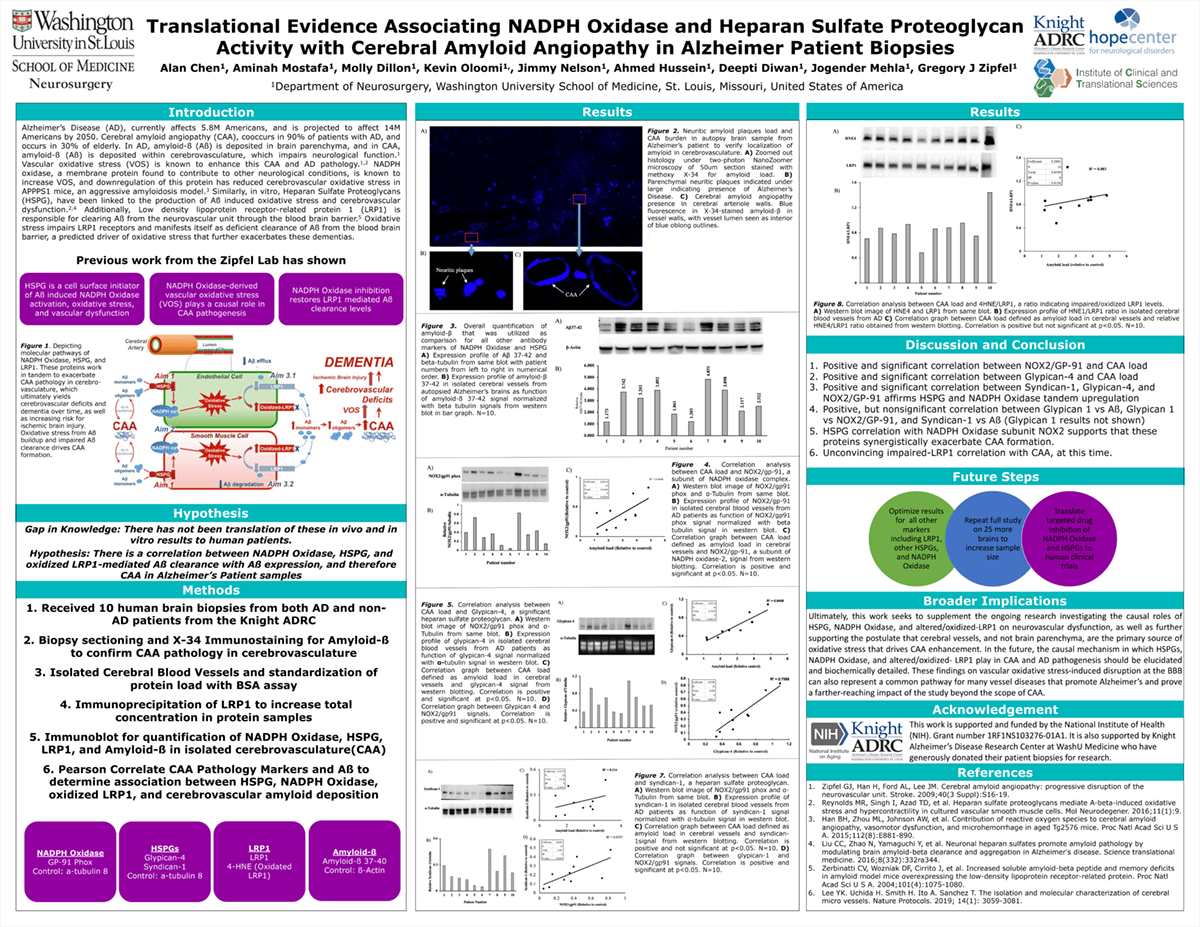
Methods: This study correlated HSPG expression and NADPH oxidase activity with each other, as well as VOS, and CAA in cerebral vessels of AD and non-AD patients, which were all hypothesized at a statistically significant positive correlation. These biopsies were digested for western blot expression analysis of NADPH oxidase, HSPG, and LRP1. Vasculature was isolated from parenchyma to study CAA specifically.
Results: Significant correlation was found between NADPH Oxidase markers for NOX2, HSPG markers for glypicans and syndecans, and impaired LRP1 signal intensity with amyloid-ß signal intensity. Further, a synergistic interplay between several oxidative stress markers was found.
Impact: These confirm the proof of concept hypothesis that Aß species upregulate HSPG expression, leading to increased NADPH oxidase expression, the primary molecular source of CAA-induced VOS, in human patients. Ultimately, this complements the studies investigating cerebral vessel dysfunction in AD and CAA development. Elucidating how these druggable targets, HSPG and NADPH oxidase, independently or more likely synergistically promote CAA pathogenesis has further provided a powerful platform for developing novel CAA-targeted therapies.
Organization: Washington University in St. Louis
Chen AX, Mostafa AF, Dillon M, Mehla J, Diwan D, Hussein AE, Oloomi K, Meron B, Vissa U, Zipfel G