Introduction: Preclinical evidence suggests that responses to IO may be enhanced through the immunomodulatory effects of stereotactic radiation therapy (SRT). We hypothesized that clinical outcomes from the National Cancer Database (NCDB) would demonstrate improved overall survival (OS) in mRCC patients receiving IO+SRT versus IO alone.
Methods: Patients with mRCC diagnosed from 2012-2016 and receiving first-line IO±SRT were identified from the NCDB. The definition of SRT was ≥10 Gy in 1 fraction, ≥20 Gy in 2 fractions, ≥24 Gy in 3 fractions, or ≥25 Gy in 5 fractions. Conventional radiation therapy was allowed in the IO alone cohort. The primary endpoint was OS stratified by the receipt of SRT (IO+SRT versus IO alone). Secondary endpoints were OS stratified by the presence of brain metastases (BM) and timing of SRT (before or after IO). Events beyond 24 months were censored. Survival was estimated using Kaplan-Meier methodology and compared via the log-rank test. Adjustments for multiple comparisons were performed.
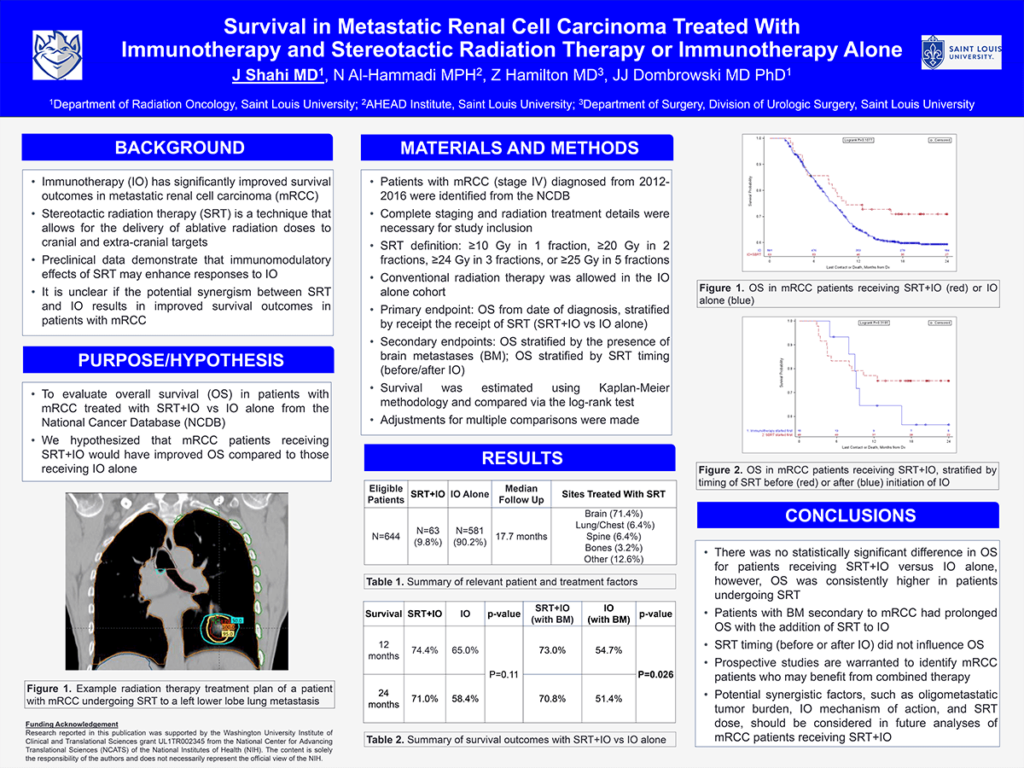
Results: Of 644 eligible patients, 63 (9.8%) received IO+SRT and 581 (90.2%) received IO alone. The median follow-up time was 17.7 months (range, 2-24 months). Baseline characteristics were similar between cohorts, although SRT+IO patients were more frequently <60 years old (57.1% vs 40.3%, P=0.010) and had higher rates of BM (71.4% vs 11.2%, P<0.001). There was no difference in metastatic tumor burden between cohorts (P=0.48). Sites treated with SRT included brain (71.4%), lung/chest (6.4%), spine (6.4%), bones (3.2%), and other (12.6%). While there was no significant difference in OS for patients receiving IO+SRT vs IO alone (log-rank P=0.11), OS was consistently higher at 1-year (74.4% vs 65.0%) and 2-years (71.0% vs 58.4%). In patients with BM, 1-year survival rates were 73.0% (95% CI, 57.4-83.7) with IO+SRT and 54.7% (95% CI, 41.8-65.9) with IO alone (P=<0.026). The timing of SRT (before or after IO) did not influence OS (P=0.32).
Impact: Patients with BM secondary to mRCC had prolonged OS with the addition of SRT to IO. Prospective clinical trials are warranted to better identify mRCC populations which may benefit from combined modality therapy.
Organization – Saint Louis University
Shahi J, Al-Hammadi N, Hamilton Z, Dombrowski JJ