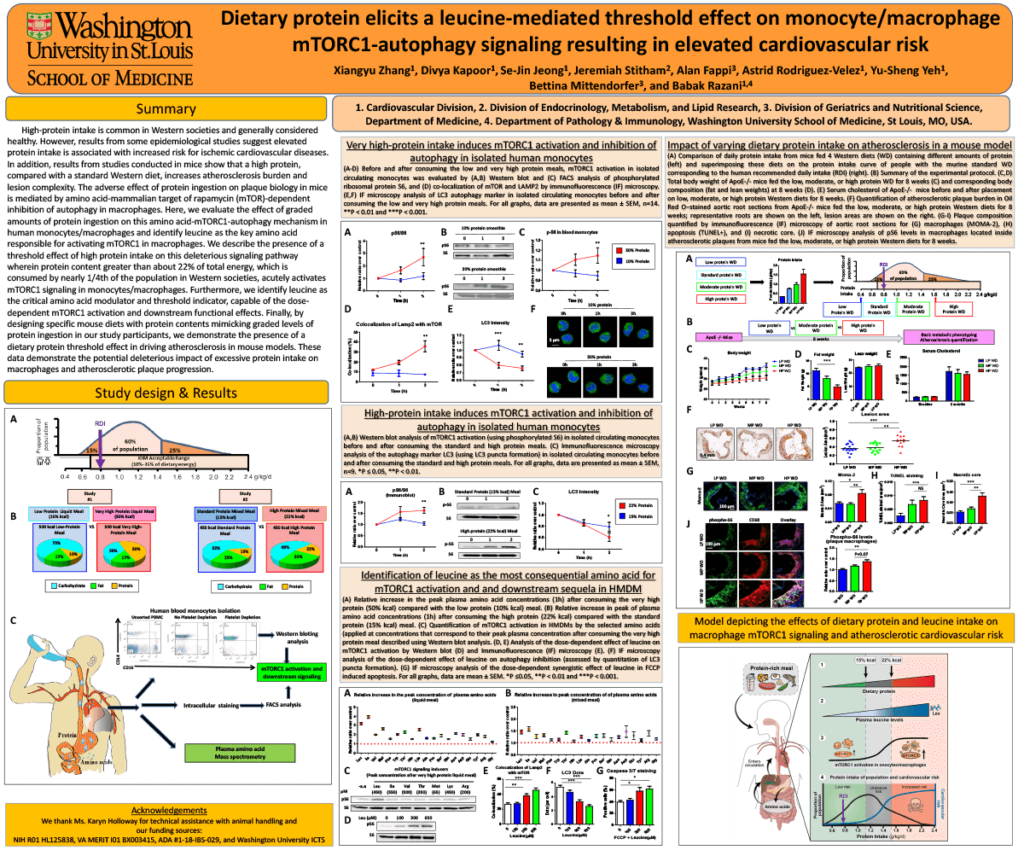
Introduction: High-protein intake is common in Western societies and generally considered healthy. However, results from studies on both participants and mice suggest elevated protein intake is associated with increased risk for cardiovascular diseases, although the dose at which protein intake can trigger mTOR activation and reach unhealthy levels and the specific amino acid(s) responsible for it are unknown.
Methods: In order to determine the effects of high protein intake on mTORC1-autophagy signaling in human circulating monocytes, we conducted two distinct clinical studies. In the first study, we evaluated extremes of protein intake by comparing the effects of liquid protein meals that contained either 10% or 50% kcal protein on monocyte mTORC1 activation in a cohort of participants. In the second study, we utilized a more “real-world” scenario, by evaluating these outcomes in participants who consumed either a 15% kcal or a 22% kcal protein meal. Circulating monocytes were isolated from blood at different time points after consuming these meals. Meanwhile, serum was also collected for detailed plasma amino acid analysis.
Results: We describe the presence of a threshold effect of high protein intake on this deleterious signaling pathway wherein protein content greater than about 22% kcal acutely activates mTORC1 signaling in human monocytes/macrophages. Furthermore, we identify leucine as the critical amino acid modulator and threshold indicator, capable of the dose-dependent mTORC1 activation and downstream effects. Finally, by designing specific mouse diets with protein contents mimicking graded levels of protein ingestion in our study participants, we demonstrate the presence of a dietary protein threshold effect in driving atherosclerosis in mouse models.
Impact: The results from the present study help explain the increased cardiovascular disease mortality associated with high protein and provide a direct mechanistic link for this association. This has important clinical and public health implications in suggesting high protein intake should be considered with caution and under corresponding guidelines.
Organization – Washington University in St. Louis
Zhang XY, Kapoor D, Jeong SJ, Stitham J, Fappi A, Rodriguez-Velez A, Yeh YS, Mittendorfer B, Razani B