The CTSA program was developed to accelerate new treatments from the lab to patients, enabled to a large extent by patients participating in and benefiting from clinical trials. Clinical trials provide that needed bridge from human subjects to hypotheses to treatments that can directly benefit human health. And, never has this connection been more critical than amid the global COVID-19 pandemic.

With the onset of COVID-19 in March 2020, many CTSAs including the Washington University Institute of Clinical and Translational Sciences (ICTS), pivoted immediately to research on SARS-CoV-2. Specimens were urgently needed to help investigators understand the pathobiology of this novel coronavirus to develop diagnostics for infection and aid vaccine efforts. During these early days of the pandemic, the ICTS acted quickly to help establish a biorepository to fill this need at Washington University School of Medicine. Rachel Presti, MD, PhD, an associate professor of medicine and medical director of the Infectious Diseases Clinical Research Unit, was one of many ICTS investigators involved in the early development of the biorepository. Along with Washington University faculty members Jane O’Halloran, MD, PhD; Charles Goss, PhD, and Philip Mudd, MD, PhD, Presti was developing plans to best collect biological samples and establish protocols to efficiently distribute specimens to the researchers that needed them.
Funding programs advance understanding of antibody response
From these early efforts, Presti realized a need to follow the donors longitudinally in order to observe their long-term immune responses after infection. At the time, the ICTS had just announced the COVID-19 Research Funding Program, an award program supporting COVID-19 translational research with potential direct clinical impact. Presti used samples from the biorepository to understand “Clinical Predictors of Longitudinal Antibody Response to SARS-CoV-2”, supported by this funding scheme. Presti and her team evaluated immune response every quarter over the first year after infection to understand who makes good antibodies, how long they last, and how protective they are. “This study was hugely successful in understanding antibody response,” commented Presti. “And it also raised a lot of questions regarding what affects that antibody response. Questions that myself and others wanted to investigate further.”
Other ICTS investigators built on the clinical discoveries from this initial antibody study. As part of Presti’s team, Ali Ellebedy, PhD, an associate professor of pathology & immunology, of medicine and of molecular microbiology, saw an opportunity to investigate the role of bone marrow in providing long-lasting antibody protection. Ellebedy, collaborating with Presti and a team of other Washington University ICTS investigators, published findings that suggested even mild cases of COVID-19 leave those infected with lasting antibody protection in the May 24, 2021 issue of Nature. This paper was also supported in part by an ICTS STAR awarded to Presti and her team in February 2021 to continue research regarding antibody responses in relation to COVID, this time post-vaccination. With her investigator team, including Ellebedy and Alfred Kim, MD, PhD, assistant professor of rheumatology, they enrolled participants to help understand the nuances of the antibody immune response to vaccination among both healthy people and those with autoimmune diseases. Presti’s efforts in obtaining key clinical data as part of this collaborative team continues to impact COVID-19 studies, including a study recently published in the June 28, 2021 issue of Nature, where ICTS researchers have found evidence that immune response to vaccines that utilize mRNA technology is both strong and long-lasting.
Interest in this research has garnered attention on a nationwide level with NIH Director, Francis Collins, MD, profiling the study in his July 13, 2021 blog post, “mRNA Vaccines May Pack More Persistent Punch Against COVID-19 Than Thought”.
Presti facilitates COVID-19 vaccine trials
Presti also took an active part in vaccine trials locally in the St. Louis area. Well-positioned to conduct vaccine trials based on her expertise in infectious disease research, Presti was tasked in the summer of 2020 with leading the effort from Washington University School of Medicine as part of the COVID-19 Prevention Network (CoVPN), a network formed by the National Institute of Allergy and Infectious Diseases (NIAID) to develop and test vaccines and treatments in the fight against COVID-19.
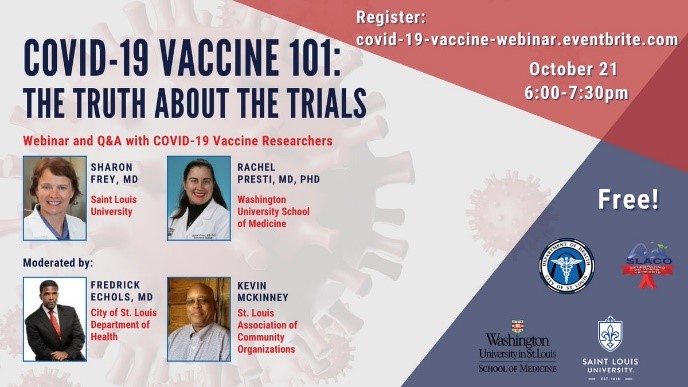
Presti worked with Sharon Frey, MD, ICTS investigator and clinical director for Saint Louis University’s (SLU) Center for Vaccine Development and principal investigator of the CoVPN trial at SLU. Together they worked to recruit participants and communicate with the public about the need for participation. Aware of how critical community support is to clinical trials, both Frey and Presti consulted with the ICTS Community Advisory Board regarding best practices for communicating with the community. That consultation helped develop their joint presentation with the City of St. Louis Department of Health, “COVID-19 Vaccine 101: The Truth about the Trials” where they discussed the ongoing vaccine studies with St. Louis City residents via Zoom.
Building bridges
From her expertise with clinical trials to her research endeavors, Presti takes an active role throughout the translational research process. “I view what I do as a translational researcher is like being a bridge, facilitating the clinical to basic science component of a study,” Presti explains. “I work to find the right patients, obtaining appropriate samples at appropriate times to get well-curated data for scientists to use to see what the predictors of response or what correlates of immunity might be. Once that link from the clinical data is built, it is truly amazing to see the science that develops from there.”
